You are here
Retinal Detachment
What is a detached or torn retina?
The retina is a layer of light-sensing cells lining the back of your eye. As light rays enter your eye, the retina converts the rays into signals, which are sent through the optic nerve to your brain where they are recognized as images. Macula is the central portion of the retina responsible for detailed vision which is needed for activities such as reading and driving.
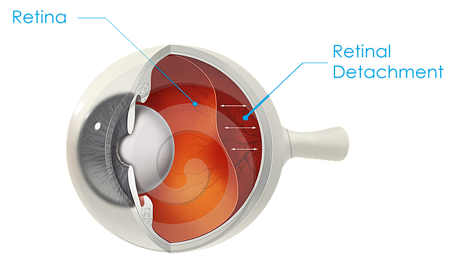
Retinal detachments will affect one out of every 10,000 people each year in the United States. Retinal detachments start as retinal tears. When retina tears are left untreated, watery fluid from the vitreous space passes through the hole and flows between the retina and the back wall of the eye. This separates the retina from the back of the eye, causing it to detach. Then the retina becomes unable to transmit the light images via the optic nerve to the brain. The part of the retina that is detached will not work properly and there will be a blur or a blind spot in vision. The most severe case is the detachment of the retina, which results in blindness. Over 90% of all retinal detachments can be reattached by modern surgical techniques. Occasionally, more than one operation may be required.
What causes retinal detachment?
Most retinal detachments are caused by the presence of one or more small tears in the retina. These tears may be due to the thinning of the retina that comes with age, but more often they are caused by the shrinkage of the vitreous. The vitreous is a clear gel that fills the middle of the eye. The vitreous helps maintain the shape of the eye and allows light to pass through the retina.
Who is at risk for retinal tears and detachments?
Retinal tears and detachments usually affect people who are middle-aged or older. These eye problems are more likely to develop in very nearsighted people and those with a family history of retinal problems. A hard, solid blow to the eye may also cause retinal detachments.
What are the symptoms of a retinal tear or detachment?
- Light flashes
- New floaters - little "cobwebs" or specks that float in your field of vision
- A gray curtain moving across your field of vision
- Sudden blurry vision
These symptoms do not always mean a retinal detachment is present; however, you should see your ophthalmologist as soon as possible. Your ophthalmologist can diagnose retinal detachment during an eye examination in which he or she dilates the pupils of your eyes. Some retinal detachments are found during a routine eye examination.
What treatment is needed?
- Retinal Tears - Most retinal tears need to be treated with laser surgery or cryotherapy (freezing), which seals the retina to the back wall of the eye. These treatments cause little or no discomfort and may be performed in your ophthalmologist's office. Treatment usually prevents retinal detachment.
- Laser Surgery - during laser surgery, your ophthalmologist will use a laser to place small burns around the edge of the retinal tear. These burns produce scars that seal the edges of the tear.
- Cryopexy - during this procedure, your ophthalmologist will use an intensely cold probe to freeze the back wall of the eye behind a retinal tear. This will stimulate scar tissue and seal the edges of the tear.
- Retinal Detachments - almost all patients with retinal detachments require surgery to return the retina to its proper position. There are several ways to fix a retinal detachment. The most common surgical procedures are scleral buckling, pneumatic retinopexy and vitrectomy. Each is designed to press the wall of the eye against the retinal holes, holding together until scarring heals the tears.
- Scleral Buckling - this treatment involves placing a flexible band (scleral buckle) around the eye gently pressing inward and holding the retina in position. This procedure is performed in an operating room.
- Pneumatic Retinopexy - in this procedure, a gas bubble is injected into the vitreous space inside the eye. As the bubble rises, it presses the detached retina against the back wall of the eye to seal the retinal tear. Your ophthalmologist will ask you to maintain a certain head position for several days. The body usually absorbs the bubble within one to three weeks.
- Vitrectomy - the vitreous gel, which is pulling on the retina, is removed from the eye and usually replaced with a gas bubble. Your body's own fluids will gradually replace the gas bubble. Sometimes vitrectomy is combined with a scleral buckle.
How safe is surgery?
Surgery is successful in preserving eyesight in more than 90 percent of patients, although a second operation is sometimes needed. The benefits of surgery clearly outweigh the risks. Some of the surgical risks include infection, bleeding, high pressure in the eye and cataract. If the retina cannot be reattached, the eye will continue to lose sight and ultimately become blind.
Home
......................................
Locations
......................................
Schedule Appointment
About
......................................
Press & Events
......................................
Testimonials
Retina Conditions
......................................
AMD - Macular Degeneration
......................................
Diabetic Eye Disease
......................................
Epiretinal Membrane
......................................
Macular Hole
......................................
Retinal Detachment
Research
......................................
Tools & Resources
......................................
Contact



